Hormone Receptor Status
Hormone Receptor Status
Samhita Vellala and Dr. Lopamudra Das Roy
Published 2020
@BreastCancerHub, All Rights Reserved
Understandably, cancer is a difficult topic to discuss. The taboo surrounding this word lends itself to simplification and subsequently generalization in our society. Many believe there is only one ‘type’ of lung cancer, one ‘type’ of pancreatic cancer, or one ‘type’ of breast cancer. This is far from the truth.
Breast Cancer is in itself a subcategory composed of multiple subgroups. The cancer may be of different grades. Diagnoses may also be categorized by Hormone Receptor Status and HER2 Status.
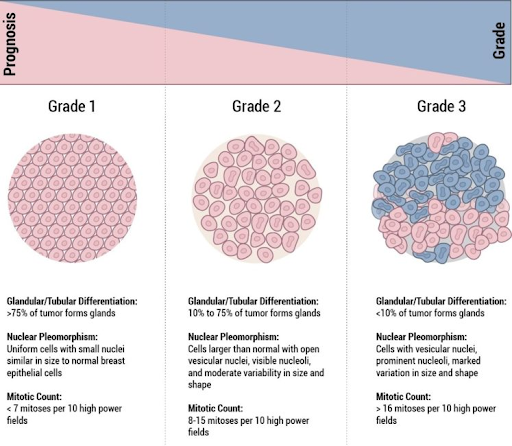
Grades of Breast Cancer (Picture Source: https://pathology.jhu.edu/breast/staging-grade/)
What are the Grades of Breast Cancer?
Grade 1
The cells are similar-looking to normal tissue and are growing very slowly. They are well-differentiated.
Grade 2
The cells are in a stage somewhere between Grade 1 and Grade 3. They are moderately-differentiated.
Grade 3
The cells are very abnormal-looking and are rapidly growing. They are poorly-differentiated.2
Hormone Receptor Status and Targeted Therapy
Depending on the individual, breast cancers can be sensitive to estrogen and/or progesterone, hormones that occur naturally in the female body. Receptors on the outside of these cancer cell walls can catch hormones circulating through the body. In addition to surgery, chemotherapy, and radiation, targeted therapy focuses on attacking a certain characteristic of a cancer cell, such as the protein allowing for abnormal cell growth. Studies show that pregnant women should not get targeted therapy.
Testing for Hormone Receptor Status (estrogen and progesterone receptors)
ImmunoHistoChemistry (IHC): Staining process to make hormone receptors noticeable by microscope in a biopsied sample of the breast cancer tissue
ER Positive Carcinoma, IHC
(Picture Source: https://pathology.jhu.edu/breast/testing)
Results may be reported in one of the following ways:
Percentage of cells that stain positive for hormone receptors per 100 cells, meaning they have hormone receptors.
Allred Score: Considers positive stain percentage as well as the intensity to which the receptors are made noticeable as a result of the staining. The scale ranges from 0 to 8. The higher the score, the more receptors were located and the greater intensity to which they were made noticeable.
Positive (cells stain positive for hormone receptors) / Negative (cells stain negative for hormone receptors)
Note: If your test result is simply positive/negative, you may ask your doctor for a more detailed result. If you test positive for these hormone receptors, hormonal therapy may prove to be an effective treatment for your cancer. They inhibit cancerous cell growth by lowering the amount of these hormones in your body or blocking their effects. If less than 10% of your breast cancer cells stain positive for hormone receptors, labs may consider the test as producing a negative or positive low result. Studies have proven that hormonal therapy may still be effective for breast cancers with a low percentage of hormone receptors. If you receive a score of 0, the cancer is known as hormone receptor negative, and hormonal therapy will probably prove to be ineffective. Make sure to ask for an explanation if your cancer tests to be hormone receptor negative; you may need to consider a re-evaluation of the results. If the hormone status is “unknown”, talk to your doctor to understand the meaning of this report and decide next steps to determine your hormone receptor status.
Here are the possible test results:
ER+
PR+
ER+/PR-
ER-/PR+
ER+/PR+ (HR+)
ER-/PR- (HR)
Estrogen Receptor Positive (ER+ or ER+/PR-)
In this type of cancer, cells use estrogen to grow by catching this hormone through receptors.
Progesterone Receptor Positive (PR+ or ER-/PR-)
In this type of cancer, cells use progesterone to grow by catching this hormone through receptors.
Hormone Receptor Positive (HR+ or ER+/PR+)
Type of breast cancer where cancer cells have one or both hormone receptors above. Using anti-progesterone hormone therapy, otherwise known as endocrine therapy, can help prevent the growth of these cancer cells.1
Popular Types of Hormonal Therapy
Aromatase Inhibitors: Prevent estrogen production in postmenopausal women only. Aromatase is an enzyme in the body which is responsible for converting the androgen hormone into small quantities of estrogen. With less available estrogen, the growth of these dependent cells is slowed. Examples of Aromatase Inhibitors include Arimidex, Aromasin, and Femara.
Selective Estrogen-Receptor Response Modulators (SERMs): Help to block the effect estrogen has on cancer cells by attaching to their estrogen receptors. One modulator commonly used to treat breast cancer patients is known as Tamoxifen.
Other Types of Hormonal Therapy
Estrogen-receptor downregulators (ERDs): Sit in the receptors of these cancer cells, so that the estrogen cannot attach to them. ERDs lower the amount of estrogen receptors, and modify their shape so they work less efficiently. Faslodex is an example of an ERD, that may be used to treat the following cases:
First treatment: HR-positive, HER2-negative, advanced-stage breast cancer in postmenopausal women.
Postmenopausal women diagnosed with advanced-stage, HR-positive breast cancer when hormonal therapy medicines fail to show continued progress.
Luteinizing hormone-releasing hormone agents (LHRHs): Hinder the function of the ovaries to prevent the production of estrogen. The agents are administered through injection once a month for a select period of time, or once every few months. Examples include Zoladex, Lupron, and Trelstar. LHRHs are effective for treating early-stage, HR-positive breast cancer in premenopausal women. Once the administration of the LHRHs is terminated, the ovaries eventually return to normal function.
If the above treatments are unsuccessful and the patient is suffering from HR-positive advanced breast cancer, the following treatments may be successful: Megace reduces the impact estrogen has on breast cancer cell growth, and Halotestin is an anabolic steroid that lowers estrogen levels in the body.4
mTOR Inhibitors: Used when Arimidex or Femara are no longer effective treatment methods. They prevent cancer cells from receiving needed energy. One such inhibitor is Afinitor.
CDK4/6 Inhibitors: Effective in treating advanced-stage or metastatic, hormone-receptor-positive, HER2-negative breast cancer. They prevent the growth and division of cancer cells. Examples include Kisqali, Ibrance and Verzenio.
PI3K inhibitors: Effective in treating advanced-stage or metastatic hormone-receptor-positive, HER2-negative breast cancer; individuals also with a PIK3CA mutation that has grown after treatment with hormonal therapy in postmenopausal women and men. One such inhibitor is Piqray.7
Prophylactic Ovary Removal: A more aggressive method of lowering estrogen levels in the body, adopted by premenopausal women. The implications of this surgery are permanent, as women will no longer be able to have biological children.4
Hormone Receptor Negative (HR- or ER-/PR-)
Type of breast cancer where cancer cells have neither of the hormone receptors above.
Treatment
Hormone therapies are ineffective.
Surgery, chemotherapy and radiation are still effective treatments. In fact, studies suggest chemotherapy may be a more effective treatment for HR- breast cancer than for HR+ breast cancer.5
What is HER2 Status?
Testing for HER2 Status
ImmunoHistoChemistry (IHC): HER2 proteins are stained in a biopsied sample of the breast cancer tissue. The IHC provides a score ranging from 0 to 3+, which represents the quantity of HER2 proteins on the cell surfaces. The cancer is known to be HER2-Negative if the score is 0 to 1+. The cancer is known to be borderline if the score is 2+, and HER2-positive if the score is 3+. If the score is borderline, the FISH test will be conducted on a biopsied sample of the breast cancer tissue to clearly determine HER2 Status.
FISH (Fluorescence In Situ Hybridization): This is a more accurate test, but is more expensive and has a longer wait time. Special labels containing chemicals are attached to the HER2 proteins. When these labels are attached to the proteins, their color changes, and they glow in the dark. The FISH provides a score of positive or negative.
HER 2-Positive Carcinoma, FISH (Picture Source: https://pathology.jhu.edu/breast/testing)
Note: Medicines treating HER2-positive breast cancers are usually only effective for cancers that test IHC 3+ or FISH positive. Over time, HER2-positive breast cancers may become HER2-negative, and vice versa. If your cancer returns as an advanced illness, a new biopsy and HER2 Status test should be ordered.
HER2-Positive
HER2 is a protein that promotes breast growth. Breast cancer cells are considered HER2-positive if they contain abnormally high levels of this protein. This type of breast cancer grows and metastasizes more rapidly than other types. They usually respond well to treatment involving the use of drugs that target HER2.
Treatment
Enhertu combines anti-HER2 medication and deruxtecan. It delivers topoisomerase I inhibitor to cancer cells by attaching the inhibitor to the medication. Through this method, chemotherapy is delivered to the cancer cells.
Herceptin prevents cancer cells from receiving chemical signals that promote growth. Similar medications include Nerlynx and Perjeta.
Kadcyla combines Herceptin and emtansine, a chemotherapy medication. By attaching emtansine to Herceptin, cancer cells receive emstancine. Herceptin delivers emtansine to the cancer cells.
Tykerb blocks select proteins that promote the uncontrolled growth of cells.6
Phesgo is an effective treatment for HER2-positive breast cancer when administered with chemotherapy. It is administered by injection, and includes a fixed-dose combination of Herceptin, Perjeta, and hyaluronidase-zzxf.
Tyrosine Kinase Inhibitors: Responsible for managing the division and growth of cells. If there is an abnormally high amount of Tyrosine Kinase in the cell, or if the enzyme itself is overactive, cells may begin to grow abnormally quickly. Tyrosine Kinase Inhibitors help to block a particular location of the HER2 gene in these cancer cells, therefore inhibiting their quick growth. One such inhibitor is Tuksya.7
What is Triple Negative Breast Cancer?
Triple Negative Breast Cancer
Type of breast cancer which tests negative for estrogen/progesterone receptors and abnormally high HER2 protein levels.1
Challenges
Seen as more aggressive, and has an extremely poor prognosis (likely trajectory of an illness), because there are fewer targeted treatments for this form of breast cancer. It is more likely to metastasize (spread to other parts of the body), and return after treatment.
It is usually of higher grade, specifically grade 3.
Cancer cells are very similar to basal cells, which line the breast ducts. “Basal-like” cancers are aggressive and high in grade as well.8
Treatment
Trodelvy: Effective in treating metastatic triple-negative breast cancer, where two previous therapies have ceased to be effective. This medication is administered directly into the bloodstream through IV or port.10
Other Treatment
PARP Inhibitors: In individuals with a BRCA1 or BRCA2 mutation, these inhibitors can be used to treat advanced-stage HER2-negative breast cancer. PARP enzymes repair DNA damage in cells. These inhibitors make it difficult for cancer cells with the BRCA 1 or BRCA 2 mutation to repair damaged DNA, reducing their chances of survival. One example of a PARP Inhibitor is Lynparza (works against metastatic HER2-negative breast cancer).7
Immunotherapy: Medications strive to increase function/efficiency of the immune system to attack cancer cells. Immune checkpoint inhibitors help the immune system to “see” cancer cells by focusing on a certain protein which “hides” them, so they are easier to kill.
T cells are immune cells. There is a protein known as PD-1 on these cells. In normal conditions, when PD-1 attaches to PD-L1 (a protein located on many normal and cancer cells), it prevents the T cells from attacking the body’s cells. Sometimes, cancer cells have excess amounts of PD-L1, which allow them to stay “safe” from an attack by the T cells. Antibodies target either one of these proteins can prevent this attachment, therefore allowing for the immune system to kill off more cancer cells. PD-1 inhibitors include Pembrolizumab (Keytruda), Nivolumab (Opdivo), Cemiplimab (Libtayo). PD-L1 inhibitors include Atezolizumab (Tecentriq), Avelumab (Bavencio), Durvalumab (Imfinzi).9
___________________________________________________________________________
It is important to understand that there are multiple types of Breast Cancer, so the correct treatment can be administered. Additionally, it is extremely crucial that patients and their loved ones educate themselves so they can advocate for the patient’s breast health, as well as the breast health of others in their community. Cancer is a complicated and frightening disease, but Breast Cancer Hub is here to help. We hope this article was insightful for affected individuals and their loved ones.
Sources
2https://ww5.komen.org/BreastCancer/TumorGrade.html
3https://www.breastcancer.org/symptoms/diagnosis/hormone_status/read_results
4https://www.breastcancer.org/symptoms/diagnosis/hormone_status/treatment_hrpos
5https://www.breastcancer.org/symptoms/diagnosis/hormone_status/treatment_hrneg
6https://www.breastcancer.org/symptoms/diagnosis/her2
7https://www.breastcancer.org/treatment/targeted_therapies
8https://www.breastcancer.org/symptoms/diagnosis/trip_neg
10https://www.breastcancer.org/treatment/targeted_therapies/trodelvy